Project MulioBio: Rethinking Psychiatric Disorders - A Shift from Diagnostic Labels to Biological Mechanisms
What if psychiatric care focused less on diagnostic labels and more on what’s really happening in the body? The MulioBio project, funded by ERA-Net NEURON’s Joint Transnational Call 2019, set out to challenge traditional boundaries in psychiatry by identifying biological markers that correlate with symptoms—regardless of formal diagnosis.
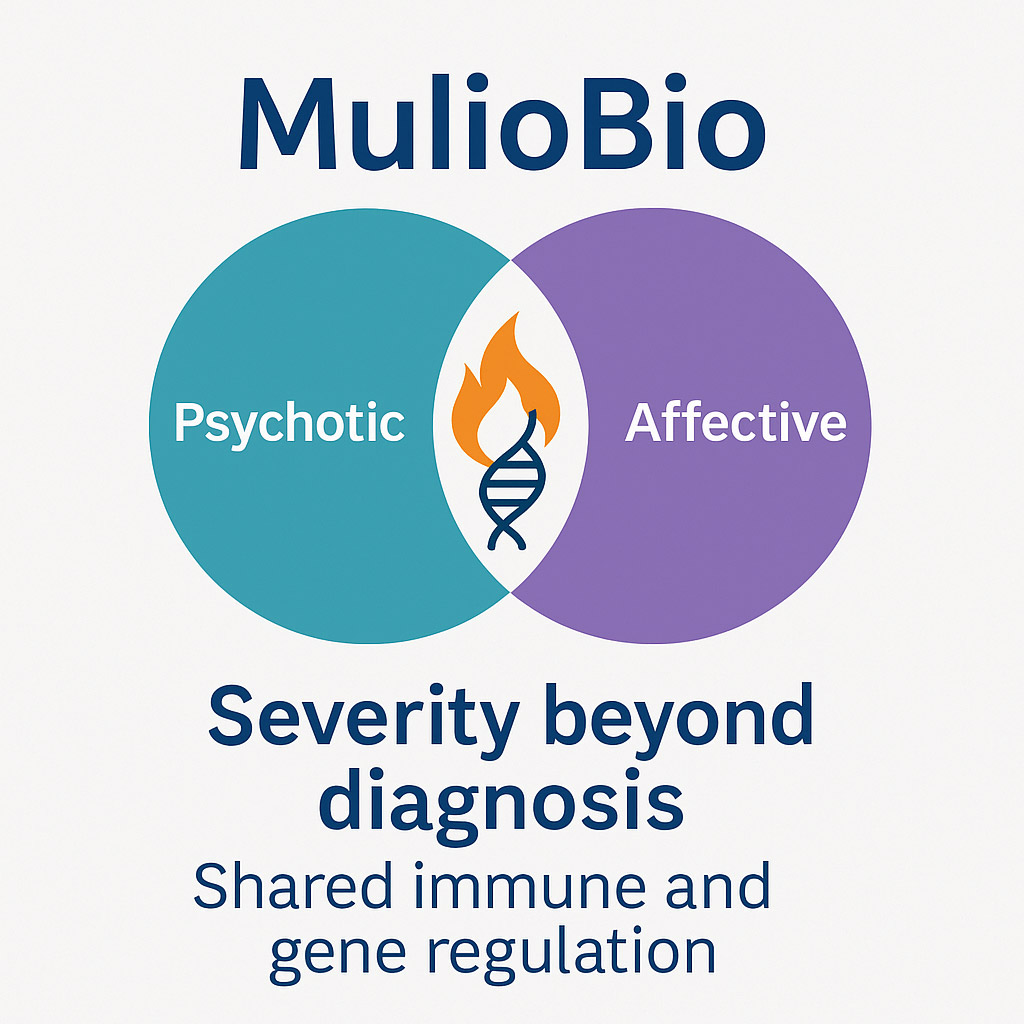
Schizophrenia and bipolar disorder are typically treated as distinct conditions. Yet in clinical practice, they often present with overlapping symptoms and biological risk factors, which complicates diagnosis and limits treatment options. Instead of relying solely on established diagnostic labels, the MulioBio consortium grouped patients according to broader symptom dimensions and illness trajectories, in an effort to uncover shared biological mechanisms underlying severe mental illness.
MicroRNA Insights into Mental Illness
One arm of the project investigated differences in gene regulation by analyzing microRNAs, small molecules that help control gene expression, in the blood of patients with varying symptom profiles. Rather than assigning participants to traditional diagnoses, the researchers organized them into two broad groups: an “affective” group, characterized by mood-related symptoms, and a “psychotic” group, marked by psychotic symptoms like hallucinations or delusions.
The analysis revealed distinct patterns of microRNA expression between these patient groups and healthy controls. Several of the microRNAs identified had not previously been associated with psychiatric conditions, offering promising new insights into the molecular pathways involved in mental illness and suggesting that microRNA dysregulation may be a biological signature of psychiatric disorders, offering new biomarkers for diagnosis and treatment. These findings were published in Molecular Psychiatry (PMID: 40263528).
Inflammation and the Severity of Illness
A second study within MulioBio examined the relationship between symptom severity and immune system activity. Patients were grouped based on the course of their symptoms over time, rather than by diagnosis. The researchers discovered that those with more severe or persistent symptoms (regardless of whether they had schizophrenia or bipolar disorder) showed elevated levels of inflammation-related proteins in their blood.
This suggests that inflammation may not be unique to a specific psychiatric disorder, but instead a shared biological driver of disease severity. These results were published in Brain, Behavior, and Immunity (PMID: 40505822).
A New Biology-Informed Perspective on Psychiatric Illness
Together, these findings support a more integrated and biology-informed understanding of psychiatric disorders—one that prioritizes shared mechanisms like inflammation and gene regulation over rigid diagnostic categories. By focusing on common biological signatures, this approach has the potential to enable earlier detection, more accurate patient stratification, and treatment strategies guided by molecular profiles rather than trial and error.
To move toward clinical application, the team is now seeking funding to validate the identified biomarkers in larger, independent cohorts, an essential step to confirm their reproducibility and predictive value. In parallel, new collaborations have been initiated to explore proteomics datasets and further characterize inflammation across diagnostic groups. These efforts aim to lay the groundwork for developing practical stratification tools that can support more personalized psychiatric care.
A Consortium Built on Complementary Strengths
MulioBio’s success was made possible by the support of ERA-Net NEURON’s Joint Transnational Call 2019, which enabled the formation of a strong multinational and interdisciplinary research consortium. The project was led by Dr. Jeremie Poschmann (Université de Nantes, CR2TI – Centre for Research in Transplantation and Immunology, France), in collaboration with Prof. Dr. Thomas Gerd Schulze (Ludwig-Maximilians-University Munich, IPPG – Institute of Psychiatric Phenomics and Genomics, Germany) and Dr. Igor Jurisica (Krembil Research Institute, Toronto Western Hospital, Canada). The consortium brought together complementary expertise in immunology, psychiatry, and computational biology, enabling the generation, analysis, and integration of large-scale biological data. While CR2TI is a leader in omics and translational immunology but not typically focused on mental disorders, IPPG contributes deep clinical insight into psychiatric illness through initiatives such as the longitudinal PsyCourse Study, though without specialization in immunological data. The collaboration between CR2TI and IPPG proved especially synergistic, allowing the integration of diverse perspectives and producing more meaningful and integrative outcomes than either institution could have achieved alone. The additional involvement of the Krembil Research Institute brought further strength in computational biology and systems-level data analysis, reinforcing the value of international and cross-disciplinary cooperation in advancing psychiatric research.
What made the MulioBio project most meaningful for me was the chance to connect psychiatric research with immunology and molecular biology, which is where my expertise lies. It was also my first experience leading a consortium, and I learned a great deal about building trust, navigating different perspectives, and finding common ground across disciplines and countries.